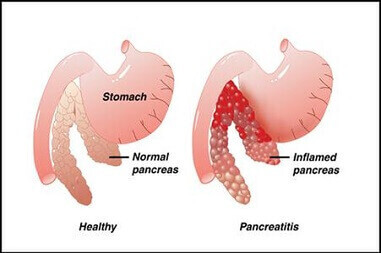
Pancreatitis is inflammation of the pancreas. If it starts to malfunction as a result, with digestive juices leaking out into the surrounding tissue, the result will be acute pancreatitis in dogs. This is extremely painful as the body begins to digests itself. Pancreatitis in dogs and cats is all too common a feature and is almost certainly a result of dry feeding.
Types and Symptoms of Pancreatitis in Dogs
Pancreatitis in dogs can be either acute (rare) or chronic (most likely). Acute pancreatitis is a crippling painful disease whereby abnormal pancreatic function causes the release of digestive enzymes into the pancreas, surrounding organs and tissue. Essentially the body starts to digest itself. At this stage it is termed necrotising pancreatitis. It has a sudden onslaught and without rapid veterinary intervention and aggressive treatment your dog is unlikely to survive.
Chronic pancreatitis takes time to develop and is thus more likely to occur in animals two years and older. It is characterised by an inability to secrete digestive enzymes. Symptoms will not appear until 85–90% of the pancreas is shut down (Ettinger et al. 1995). Fewer enzymes mean less fat and protein being digested. These undigested fatty acids in the gut causes the diarrhoea which is yellowy-grey and oily in nature, typical of this disease. Symptoms are not as violent as in acute pancreatitis and are associated with the lack of digestion, including weight loss, poor hair coat, flatulence, increased appetite, coprophagia (poo eating as a result of nutrient deficiency coupled with the more nutritious stools) and diarrhoea.
Prevalence of Pancreatitis in Dogs and Cats
In a study of 73 dogs presented for post-mortem examination, 64% of pancreata displayed evidence of chronic pancreatitis (Newman and Woosley 2004). The very same is seen cats. Examination of 115 feline pancreata from healthy and sick cats found pancreatitis in 67% of cases, including 45% of apparently healthy cats (Owens et al. 1975, Macy 1989, Steiner and Williams 1997, De Cock et al. 2007). Dogs and cats suffer pancreatitis to a disgracefully large degree, 25 – 50 times more than as is seen in humans (worked out from rates of dog pancreatitis in Panagiotis et al. 2008). This is as much unnatural as it is disgraceful, considering how painful the issue is for the animal.
The Likely Cause of Pancreatitis in Dogs
There are a few suspected causes but there is one certainty. Genetics is thought to play a role. For example, German shepherds can constitute up to two-thirds of Exocrine Pancreatic Insufficiency (where the pancreas is unable to produce enough of a specific enzyme, Kim et al. 2005), with rough collies, Yorkshire and silky terriers, dachshunds, miniature poodles and cocker spaniels also noted to be at risk. However, as genetics does not explain the shockingly large amount of pet cats that suffer pancreatitis, where pedigree inbreeding being less of an issue here, it is down the list of concerns.
Various infections can cause trouble in your pancreas resulting in a bout of acute pancreatitis, including Salmonella and Legionella, to name but two. But a chronically sick gut can also cause problems, where leaky gut can spread not only inflammation but pathogenic bacteria to the pancreas.
A lesser known cause of pancreatitis is injury to the mid-back (where the thoracic and lumbar vertebrae meet). This is an energy point here that supplies both the stomach and the pancreas. To check for an issue here, you don’t need an expert. You simply need to prod around where you see the last rib is coming from as it’s attached to their last thoracic vertebrae, it then becomes the lower back (lumbar vertebrae). There will be discomfort when you hit the spot. Injury or stress here is also thought to be a predisposing factor for bloat.
But all these factors are expected to pale in significance to the most common cause of pancreatitis in dogs and that is FOOD. Pancreatitis has a strong nutritional basis, certainly in human nutrition so it follows that it must play a role in dogs too. As 8/10 of our dogs today are fed completely unnatural cereal-based food it is most certainly a chief suspect.
Why High Carbohydrate Dry Food Causes Most Of The Pancreatitis In Pets..
What you will never hear from a conventionally trained vet is that dry, ultra-processed HIGH CARBOHYDRATE pet food is causing the plague of pancreatitis in our pets. They do not learn this in college, only how to suppress the symptoms when they appear. I don’t mean to be unfair but that they blame fat for causing a bout of pancreatitis (and then recommend a low-fat but HIGH CARB diet) is all the evidence we need that our vets are sadly and dangerously missing the very big picture here.
To explain why carbs are the chief suspect in pancreatitis in dogs and cats you first need to understand why fat builds in the blood.
Hyperlipidaemia (excess fat in the blood) is one of accepted causes of acute pancreatitis or recurring bouts of acute pancreatitis in humans. It is thought to account for 7% of cases, making it the most common cause of the disease after gall stones and alcohol.
The presence of excess fat is how your vet typically diagnoses the condition in your dog. A pancreas in trouble does not digest fat very well. Hence, one way to detect the possible signs of pancreatitis is to simply measure the amount of triglycerides (fat) in the blood. Another way is to test for lipase, the enzyme secreted by the pancreas to digest fat. A stressed pancreas is assumed to produce much more of it, something a simple blood test in a fasted dog would reveal. Finally, as most pancreatic dog owners will testify to, the most obvious outward sign (asides pain, as it really hurts) is a loose stool that is greasy with undigested fat.
So concerned are our vets for fat, that when discussing a possible cause of the issue the line “it can be something as simple as that bit of fat off your steak” is often trotted out. Like when we thought eating fat made you fat (giving rise to low-fat and thus HIGH SUGAR diets, greatly exasperating the obesity epidemic), it made perfect sense. If there is too much fat in the blood, then surely you have been eating too much of it. Only that statement is not only entirely unsupported by the literature but, as we have since learned from the obesity epidemic, very likely to be absolutely false. Of course, dogs should be able to eat a big lump of fatty meat now and again, that’s what they are designed to do. As you will learn below, they are more adept at utilising fat than we are.
To understand a little more about this we need to first discuss the three different energy pathways…the first is your already formed and stored energy, ATP (adenosine tri phosphate, you might remember from school!). This energy system is ready to go. As such it is rapid but short lasting. In gym terms, it can produce lots of power but only for a very short duration, perhaps twelve seconds of maximal effort. Think of it as the favoured pathway of your 100m sprinter, for instance.
The second system is known as the Glycolytic System. This system runs on glycogen (blood sugar) stored in the muscles and liver, which you create after consuming carbohydrates and, to a lesser degree, protein. In gym terms, this pathway provides for you moderate power of moderate duration, perhaps thirty seconds.
The third system is known as the fatty acid Oxidation System. This is essentially three systems (of which the Krebs cycle is part of it…I know you remember….!). For now, all we need to note is that instead of blood glycogen it uses stored fat (lipolysis) to fuel the ATP conversion. In gym terms, it offers the least power but the greatest duration. It is why top long distance runners (and all long-pursuit animals such as dogs and wolves) all do it on fat (and why they are all bordering-skeletal).
It happens that the more carbohydrates you consume, the less likely you are to use the fatty acid Oxidation System. In humans, the ingestion of high-carbohydrate diets for a long period of time decreases fatty acid oxidation by decreasing the rate of fatty acid entry into the mitochondria. This means, rather paradoxically, the more carbohydrates you consume, the less fat is consumed by the mitochondria and the net result is an elevation of blood fat. In other words, it is a high-carb diet that raises your blood fat. Authors note, that when the content of dietary carbohydrate is elevated above 55% of ME, blood triglycerides rise. It even has a catchy name too – carbohydrate-induced hypertriglyceridemia.
Studies show this is very much what’s happening in dry fed dogs. Raw-meat-and-bone fed dogs (very low carb diet) exhibited reduced blood fat than dogs fed a dry, cereal-based diet. Dr Mark Roberts is a leading authority on the role of dietary fat in dogs, particularly in relation to sporting dogs. His latest work dispels the mythological role of dietary fat in pancreatitis in dogs. They found that their dogs’ pancreas were not working harder on high-fat diets by any measure available to them. Using twenty dogs that were fed regular diets and then alternatively fed high-carb or high-fat diets, then blood fat, lipase and stool quality was measured. Roberts found blood triglycerides were not higher in the high-fat diets, as expected by conventional veterinary medicine, but actually lower than those on high-carb diets. The pancreas does not produce more lipase under a high-fat challenge but the same as a high-carb diet. Even stool quality is better in the high-fat fed dogs. Thus, by all measures, increasing dietary fat failed to induce the parameters linked to pancreatitis in dogs which conventional veterinary medicine say it does.
In short, if blood fat is an accepted cause of pancreatitis and we know high-carb diets increase blood fat, perhaps they should ease off the carbohydrates in dogs.
It gets worse for dry-fed dogs suffering pancreatitis on their high-carb meals. Once it sets in, pancreatitis will result in a Vitamin E deficiency. Vitamin E’s primary role is as an antioxidant, mopping up excess fats in the system. As the failing organ struggles to break down fat in the diet, more Vitamin E is required to clean up the excess fat. But Vitamin E is notoriously unstable. And in dry pet foods, after just six months’ storage, it is proven to reduce by 30%. It is, therefore, expected to be in short supply in most dry foods. And as this is what dry-fed dogs receive in the way of fresh nutrients, thus begins a vicious circle.
As fat builds in the blood of dogs consuming high-carb diets, the body screams for more lipase to get the fat out of the blood and the pancreas complies. Measure the dog for lipase at this point and the values will be worryingly high. What do conventional vets recommend now? Low-fat (and thus higher carb) diets. It is at this near-breaking point that, one more load of fat might push the system over the pancreatic cliff. In a perfect straw-camel’s-back scenario, it’s not the final piece of straw but the heavy load already in place. Of course, the carnivore’s pancreas should have been able for that bit of fat, as meat-eaters dogs are better as its digestion than we are (later). Sadly, it is at this low moment that modern vets tend to blame the owner for a dietary indiscretion, when it was far more likely that the vets’ own poor dietary advice put the dog on the table in the first place.
Now we have to set about fixing it.
At this point, some vets recommend a low-fat diet for a dog with pancreatitis. If your dog is right in the middle of an acute bout of pancreatitis, where excess fat has built in the blood to the point he’s nearly poisoning himself, then yes, you might feed a low fat diet (although a long period of starvation would be good advice here too as this reduces the stress on the organ more than anything). However, we are talking more long term here. We are talking about dogs with chronic pancreatitis, by far the most common sort of pancreatitis or simply dogs living with the threat of pancreatitis following an acute attack. For these dogs, the diet advice is NOT a low-fat diet but even more importantly is that you feed LITTLE TO NO CARBS.
Step 1: A Period of Digestive Rest
Fasting is good for dogs. It reduces inflammation which is good news for dogs with inflamed pancreatitis. More than that it gives the pancreas a rest. If your dog is suffering from the condition you need to avoid overstimulating the organ. Don’t poke the bee hive. So, before the new diet is employed he needs a period of digestive rest. You should starve the dog for 24hrs (48 hours in the case of acute pancreatitis). The dog will do this likely himself, it’s that sore. Starvation immediately eases the burden on the pancreas. But into the future we keep this principle in mind and reduce their meal sizes for a time. Meals need to be smaller, more often (3-5 times a day) and easily digestible. This last bit highlights the importance of fresh, unprocessed and thus easily digested food. No dry or canned foods bought in pet shops or vets. Definitely no pet store treats. Nothing with a picture of a dog or cat on it.
Step 2: Remove All Aggravating Factors
Don’t poke the bee hive. You need to address all the things that might drive inflammation in your dog in the background. The list is long. First to go is dry dog food and pet store treats. All that preserved junk. Studies show dry fed dogs undergo TEN TIMES more inflammation that raw fed dogs. .
Even anti-inflammatories and steroids are to be questioned once a week or two into his new diet plan (under the supervision of a natural vet that understands fresh nutrition) as they essentially put the repair process on hold. However, in the case of acute pancreatitis, whatever keeps the poor guy comfy until that bout passes.
Step 3: The Ideal Food for a Dog With Pancreatitis is Based on Their Natural, Diet…
Dogs evolved to eat a lean diet. Fat rabbits get eaten quicker. If we take a rat or rabbit as the average dog meal and suck all the water out, these animals are roughly 80% protein, 10% fat. So now more than ever it’s time to feed him as he is supposed to be.
Best Home Made Recipe for Dog with Pancreatitis is…
Recipe wise, the folk at the top say nothing really changes for the dog with chronic pancreatitis. It is the removal of carbs that will fix his blood fat readings. So, I advise that you aim to produce a high protein, moderate to low-fat meal, like what all dogs should be eating.
This often means easing off the beef and lamb (these meats, when fed to dogs, are usually very fatty) in favour of low-fat meat pieces such as chicken or turkey initially, at least until we get him back to normal. Non-oily fish (whitefish) too is excellent and game meats such as venison if you can source it.
As always, I recommend you make it to a ratio of 5:1:1:1, that is 5 parts meat muscle, 1 part organ (and a good variety of organs here), 1 part raw bone and 1 part veg bits, for reasons that will become clear in the article above should you be new to the raw game.
Why feeding pancreas to a dog with pancreatitis is so important…
An important nutritive concept, certainly in dogs, is like feeds like. Dogs are easy animals to feed, they work like lego. Muscle builds their muscle, cartilage feeds their cartilage, bone supports their bones, liver nourishes their liver. It follows that when an organ is in trouble, you should feed lots of that organ not only to give the dog all it needs to rebuild the organ but the dog can avail of all the extra bits therein.
A horrible experiment on dogs in the 1920’s produced a vital piece of information. They were studying diabetes and seeing what effect a new chemical called insulin had on dogs with no pancreases (say no more). They separated the dogs into two groups. To one they fed their normal food and injected them with insulin. To the others they fed raw pig pancreas along with their meal. Incredibly, the second group not only did better, needing significantly less insulin but lived significantly longer.
Sadly, once they understood insulin they threw away such findings, not a whole lot of profit in feeding pancreas.
The reason the dogs did better is that the pancreas is not just meat. It contains a natural source of insulin (as it produces it). It also contains digestive enzymes (because it produces them) which the dogs can take and use to reduce the workload of their own pancreas. It also contains glucagon and a whole host of peptides that the dog can use to help heal his own pancreas.
So go to your butcher and get some pancreas off them, doesn’t matter which animal. You need to find the butcher who is slaughtering their own animals. This would be a great addition, but only in small amounts, around 5% but dropping to 3% after he’s out of the danger zone.
Unfortunately, fresh pancreas is proving very hard to find. It’s a fatty organ, often discarded by meat producers. As such, very few producers include it in their mixes or on their website.
Natural Additions I Strongly Recommend to Help Pancreatitis in Dogs…
Digestive Enzymes
I strongly recommended the digestive enzyme mix of lipase, tripase and amylase for a pancreatic dog. The human versions are fine. These are particularly important if your dog is suffering from exocrine pancreatic insufficiency (EPI) as they will give the pancreas less work to do. Dose him according to size, sprinkle on food. If feeding actual pancreas this step is unnecessary.
Probiotics
I recommend you include some canine probiotics in their diet for at least a month while we get him right. They will help reset their digestive system, which will be in disarray. A healthy gut flora is a healthy animal and it’s not to be forgotten. Full-fat probiotic yoghurt or the likes of kefir are good additions, aiding the digestive process, but we’re unsure just how much get through the dog’s strong digestive acids. Better again would be specific canine probiotics as they’re not only tailored specifically for dogs (who have different gut flora to us omnivores).
Vitamin E & C
As the previous articles highlighted, EPI will often result in a Vitamin E deficiency as undigested fat builds in their system so you need to add some in.
A 20kg / 50lb dog would need around 400 IU of vitamin E (and around 500mg of vitamin C while you’re at it). Human types fine as long as nothing else added.
Omega 3
Omega 3 fatty acids are excellent at reducing inflammation. The ACVN recommend a therapeutic dose of 700mg of combined EPA and DHA per 10kg of dog to help alleviate some of the more painful symptoms of pancreatitis but I would keep it going in to help avoid its occurrence in the future. Careful with fish oil, a lot of crap out there. I always recommend spending a bit more, get some of the refined stuff too so the EPA/DHA content is higher. That’s what you want. You will see the cheaper types have little of this.
Golden Turmeric Paste
As always, one of the most powerful natural anti-inflammatories you can make is GTP. It’s unreal and easy to make at home. Warning: it is so effective you can’t give it with any anti-inflammatories give by the vet. Wait till the unnatural ones are not going in, I fully expect this to work as well. It will help in bad times but, like omega 3, a very small amount can be given as a maintenance dose to help avoid a bout in the future.
Will He Recover?
Yes, they absolutely can and do, providing you take evasive action now. Our experience is showing that the gross amount of pancreatitis dogs and cats are mysteriously suffering today is entirely localised in the dry-fed community. The issue evaporates once fed an appropriate fresh diet and cut out all the products. Enzyme readings return to normal after a few months. The pancreas is expected to make a recovery and clients have these dogs back eating all the usual foods a normal healthy dog will. So hang in there, you’re giving him the best fighting chance.
Dr Conor Brady